A retired nurse from Fisher Branch is raising awareness of the opioid crisis in the Interlake and beyond in order to educate people about addiction issues and show substance users that there’s hope for recovery.
Darcy Truthwaite worked as a nurse for 30 years, and in the last 16 months before she retired, she helped set up and run the Substance Use Disorder Clinic at the Percy E. Moore Hospital in Hodgson to help people who are desperate to deal with their addiction.
Since 2016, people dying from opioid toxicity in Canada has increased, said Truthwaite. And people need to know how addictive opioids are and how hard it is to get off them. That’s why she’s focusing on educating people about the drugs.
“I think a lot of my patients started using street drugs because they had no idea of the long-term effects of opioids,” said Truthwaite. “Once they became addicted, they’d have horrific withdrawal symptoms and powerful cravings, and they had no idea this was going to happen to them.”
To help raise awareness of how serious opioid addiction is and to educate people about where to get help, Truthwaite has been giving presentations to various communities in the Interlake. As president of the Toastmasters in the Arts Club, she is well versed in speaking before audiences. She recently visited Fisher River Cree Nation and also presented in Jackhead First Nation and at the Jackhead school. She has already given three presentations at Fisher Branch Collegiate to students in grades 9 to 12.
Truthwaite said there are around 200 different kinds of opioids. People are probably familiar with commonly prescribed opioids such as codeine, which is found in Tylenol 1, 2 and 3. Other opioids include oxycodone (e.g., Percocet), which became the poster child of addiction, morphine, heroin, hydromorphone, fentanyl and carfentanyl (carfentanil), which is used in veterinary medicine to tranquilize large animals such as elephants.
Opioids produce pleasant effects such as pain relief, euphoria and sedation, but they can also cause low blood pressure, loss of consciousness and suppression of breathing.
And with MRI imaging, Truthwaite said it’s possible to see physical changes in the brains of people who use opioids. There is decline in white matter which can affect learning and decision-making, the processing of new information and adapting to new circumstances.
“It also affects the cerebral cortex, which is responsible for regulating emotional impulses and making rational decisions,” she said. “Studies have shown that once addiction develops, voluntary control is reduced.”
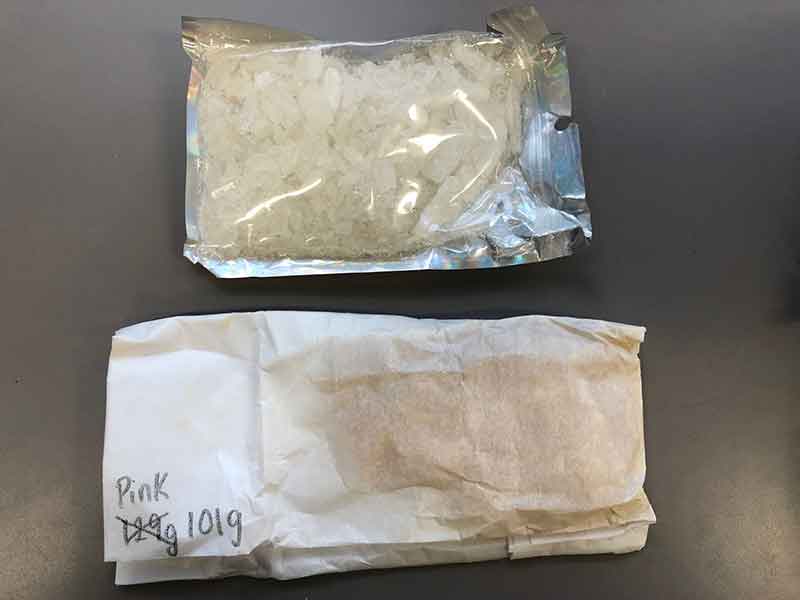
Truthwaite said all opioids can be made in illegal laboratories in Canada. Fentanyl and carfentanyl can be used as “fillers” in other drugs because they’re easy to get, cheap and make those other drugs stronger and more addictive.
If someone had a prescription for an opioid from their doctor and were then cut off, they may turn to drug dealers on the street.
Addiction usually starts by taking pills. When someone becomes tolerant to a certain level of the drug, they’ll start to crush and snort the pills, said Truthwaite. Then they’ll take it up a step by smoking it and eventually diluting and injecting it.
Once hooked, people suffer from physical and mental anguish as they crave the substances.
“It’s horrible. I found obituaries of three people who were addicted, and I refer to these obituaries in my presentations,” said Truthwaite. “One mentioned how addiction literally took over the life of one woman’s daughter. The mother said, ‘It consumed her life like a black hole and it had taken over her life. She frantically and relentlessly sought help. Nothing succeeded. Relapse always followed.’ This shows how horrible addition is. It’s been described as the worst flu ever [when people are withdrawing]. They’ll have everything from bone and joint aches to muscle spasms and twitches, goosebumps all over their body, nausea, vomiting, diarrhea, and they’ll feel restless, anxious and irritable.”
She said it takes at least 10 to 20 days of withdrawal before these symptoms abate; that depends on how long someone’s been taking opioids and how much they’ve been taking.
“It feels worse to come off opioids. A lot of my patients were on it for 10 years,” said Truthwaite. “And they didn’t know how to get help.”
Thirty per cent of opioid overdoses are linked to suicide because they “don’t know of any other way out,” she said. She researched statistics showing the growing crisis in deaths from substance abuse.
Between January 2016 and March 2021, there were 22,828 deaths (Canadians) from opioid toxicity. And Indigenous peoples identify as being “disproportionately” harmed by opioids; opioid deaths occur three to seven times more frequently than in non-Indigenous people.
“A lot of deaths are being blamed on fentanyl and carfentanyl. And today there are other drugs being thrown in the mix like the Zombie drug xylazine,” said Truthwaite.
Xylazine is an animal tranquillizer. It does not respond to naloxone, the drug that reverses opioid overdoses. Xylazine has been reported in B.C., Alberta and Ontario. Users can suffer blackout states and develop rotting flesh.
“One of the main things I want to get through to people is that when you buy drugs off the street, you never know what you’re going to get,” said Truthwaite. “I heard one report in the media of a fellow who snorted cocaine and suffered an opioid overdose – cocaine is not an opioid. It turns out the cocaine was laced with enough carfentanyl to kill eight elephants.”
The Substance Use Disorder Clinic at the Percy E. Moore Hospital, a federal hospital, can treat people addicted to opioids on a walk-in basis. However, the clinic does prefer people to call ahead so they it can ensure there’s a doctor available. In addition to medications used to help people get off opioids, the clinic provides counselling, social worker services, referrals and screening for HIV and hepatitis, which can be acquired through substance use by sharing paraphernalia such as straws or needles.
“When I retired, I was lucky to have Amanda Mann take over the clinic. She works as an addiction nurse and she’s amazing. And they just hired another nurse, Tracy Sinclair,” said Truthwaite. “There are five doctors at Percy Moore that can prescribe a treatment for opioid use disorder.”
The clinic, which opened in 2021, is provincially funded, she added, but it is not a RAAM (Rapid Access to Addictions Medicine) clinic like the one in Selkirk. It is also not a detox centre.
“For opioids, we have drugs that can stop the symptoms within 20 minutes. We mostly use suboxone, which stops the withdrawal symptoms and stops the cravings. But we have to adjust the dose and it takes about three days to adjust it on an out-patient basis That’s what the Percy Moore clinic focuses on,” said Truthwaite. “But a lot of times, people are addicted to more than one substance. So we can stabilize them on suboxone then send them to rehab to get off the rest of the substances. Unfortunately, there’s no medication for methamphetamine or cocaine. But there are medications for getting off alcohol.”
Truthwaite said she became close to her patients when she was working at the clinic and is “very proud” of all of them.
“They did well on suboxone and started changing their lives,” she said.
To contact the Substance Use Disorder Clinic at Percy E. Moore Hospital in Hodgson, call (204) 372-6906.
The clinic helps people 18 years and older. No referral is needed. The clinic does not treat people who need urgent medical attention for conditions such as psychosis, hallucinations and paranoia or who are at active risk of harm.